Imagine going to bed in a cool, dark, and quiet bedroom on comfortable sheets. After a long and peaceful slumber, you wake up — but you’re no longer in your bed.
Instead, you’re standing in the middle of the kitchen. Or you’re in the hallway, and your concerned partner is standing a few feet away from you, calling for you to wake up. Or maybe you’re even in your backyard — still wearing your pajamas.
To many people, these scenarios sound laughable. But these types of occurrences are something that people who sleepwalk have to deal with, sometimes on a regular basis.
[Editor’s Note: The content provided on this site is for general informational purposes only. Any information provided is not a substitute for professional medical advice. We encourage you to consult with the appropriate health expert if you have concerns.]
What Is Sleepwalking?
Sleepwalking is a medical condition formerly known as somnambulism. People with somnambulism will walk around or perform tasks while they are asleep. Sleepwalking isn’t just something that happens in horror movies. It’s a very real condition that, according to one study, affects over 8 million American adults each year.
In pop culture, sleepwalkers are either the butt of a joke or possessed by something supernatural. The truth is far less sensational: Sleepwalking is a relatively common phenomenon, and there’s nothing spooky about it.
In spite of the fact that it’s fairly common, sleepwalking is widely misunderstood. That’s partly because there are a number of things that could cause it, and there’s no one proven cure for it.
How Common Is Sleepwalking?
It is difficult to assess how many people actually sleepwalk. This is mostly because sleepwalkers do not always remember their nighttime episodes. While some sleepwalkers may awaken other people in their household, this is not always the case. If no one is there to witness the sleepwalking, it is hard to establish how frequently it occurs.
Still, back in 2012, researchers from the Stanford University School of Medicine estimated that 3.6 percent of U.S. adults (or more than 8.4 million people) had sleepwalked at least once in the previous year. That study, which was published in the academic journal Neurology, surveyed 19,136 individuals about their sleep and sleepwalking habits.
Smaller studies have reported different numbers. One study surveyed 228 adults in Southwestern Nigeria and found that that seven percent of respondents had experienced sleepwalking at least once in their lifetime. Another study surveyed 532 Australian teenagers and found that 2.9 percent of them recalled sleepwalking within the past month.
A review of research from 2016 collected data from 51 different studies. The combined sample was 100,490 people. The researchers concluded, “The meta-analysis showed the estimated lifetime prevalence of sleepwalking was 6.9 percent. The current prevalence rate of sleepwalking—within the last 12 months—was significantly higher in children (five percent) than adults (1.5 percent).”
Even though there’s no definitive data on how common sleepwalking is, what we do know is that millions of people will sleepwalk at some point in their lifetimes. Researchers are also fairly confident that sleepwalking is more common among children than among adults.
Sleepwalking Symptoms
Of course, the most common symptom of sleepwalking involves experiencing sleepwalking episodes, which occur when a sleeping person walks around or completes other tasks. These episodes may take many forms, but some sleepwalking activities are more common than others.
According to the American Academy of Sleep Medicine (AASM) Sleep Education website, someone who is sleepwalking might:
- Get out of their bed and walk around the room or house
- Sit up in their bed and open their eyes
- Have a glazed, glassy-eyed expression on their face
- Complete routine daily tasks
- Be difficult to wake up
- Act confused
- Quickly go back to sleep
- Not recall what happened at all
- Experience sleep terrors
In very rare cases, the AASM says, a sleepwalker could:
- Leave their house
- Get into and drive a car
- Engage in sexual activity without realizing it
- Injure themselves
- Become violent
- Engage in unusual behavior (such as urinating in a closet)
According to MedlinePlus, the time that someone spends sleepwalking can vary. A sleepwalking episode can be very brief, lasting just a few seconds or minutes, or it can last for 30 minutes or longer.
It’s common for a sleepwalker to:
- Walk around while asleep
- Open their eyes while asleep
- Speak out loud
- Raid the fridge for a late-night snack
- Be difficult to wake up
- Not remember the sleepwalking episode, especially if they go back to bed without waking up
According to the American Sleep Association, “Sleep eaters… tend to eat foods high in calories or sugar, and may eat foods while sleep-eating that they normally would not eat on their own, or which would not be seen as socially acceptable to eat on their own, such as peanut butter on its own, or sugar or syrup on its own.”
It’s less common for a sleepwalker to:
- Drive their car while sleeping (this is extremely dangerous)
- Have full conversations with other people that make perfect sense
- Engage in sexual activity while they are asleep
- Injure themselves, for example by tripping and falling, or even jumping down a flight of stairs or out of a window
Potential Risks Associated With Sleepwalking
Someone who is sleepwalking is not aware of what they are doing, which can potentially prove hazardous. For example, a sleepwalker might:
- Leave their bedroom and home entirely. This could lead to them getting locked out or exposing themselves to harsh weather.
- A sleepwalker could potentially hurt themselves accidentally. Someone who sleepwalks may trip over objects, fall down the stairs, or even jump out of a window.
- A sleepwalker could harm other people by accident. They may become aggressive and accidentally hurt someone nearby.
What exactly are the benefits of getting more sleep? See our full rundown in THIS article!
Sleepwalking And Stages Of Sleep
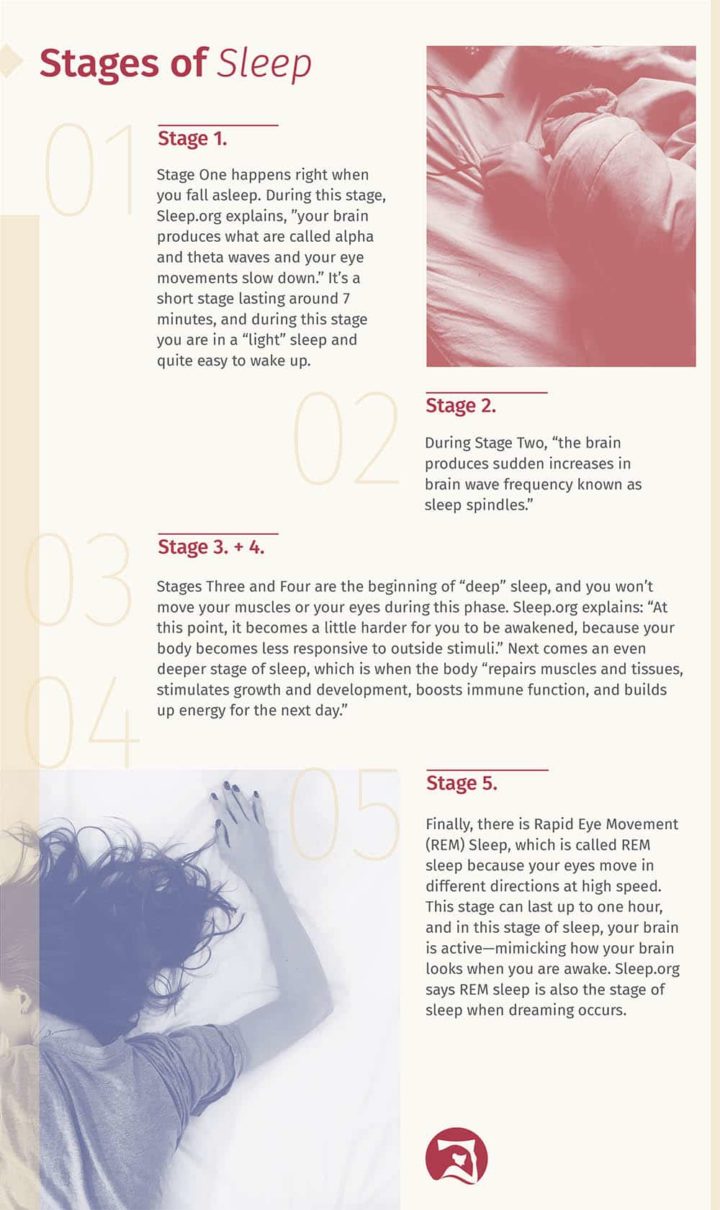
Everyone cycles through different stages of sleep multiple times during the course of a regular night. Typically, each full sleep cycle will last 90 to 110 minutes. Research suggests sleepwalking may be more common during some of these stages and less common during others.
As a general rule, sleepwalking does not happen during REM sleep. According to Psychology Today, it commonly happens during Stage 3 or Stage 4 sleep.
“The American Academy of Sleep Medicine divides our sleep time into two categories—REM sleep and non-REM (NREM) sleep, depending on whether REM (rapid eye movement) is occurring underneath the eyelids,” a Smithsonian Magazine article explains. “During REM sleep, the brain’s neuronal activity is most similar to when it is awake, and that’s when we do most of our most vivid dreaming. Paradoxically, though, sleepwalking occurs during NREM sleep.”
MedlinePlus states that sleepwalking commonly occurs during a phase of non-REM sleep that happens quite early in the night, usually within the first third of your time asleep.
What Causes Sleepwalking?
A number of different factors could cause a person to sleepwalk. The Mayo Clinic says that common causes for sleepwalking include sleep deprivation, stress, fever, and disruptions to one’s sleep schedule, like travel. Here’s a more detailed look at some of the potential causes of sleepwalking.
1. Sleepwalking could be linked to certain health conditions.
According to WebMD, certain conditions may increase the likelihood of sleepwalking. These include heart rhythm problems, fever, heartburn, nighttime asthma, and restless leg syndrome.
One study found a connection between migraine headaches and sleepwalking. Meanwhile, MedlinePlus links sleepwalking to seizure disorders and notes that, “In older adults, sleepwalking may be a symptom of a medical problem that causes decreased mental function neurocognitive disorder.”
2. Certain mental health conditions may be associated with sleepwalking.
An article about the 2012 Stanford University School of Medicine study explained that, according to those findings, “People with depression were 3.5 times more likely to sleepwalk than those without, and people with alcohol abuse/dependence or obsessive-compulsive disorder were also significantly more likely to have sleepwalking episodes. In addition, individuals taking SSRI antidepressants were three times more likely to sleepwalk twice a month or more than those who didn’t.”
Meanwhile, WebMD states that a higher chance of sleepwalking may be associated with psychiatric disorders such as post traumatic stress disorder (PTSD), panic attacks, and dissociative states such as those that characterize multiple personality disorder.
The exact nature of the connection between these various health conditions and sleepwalking is not fully understood.
“There is no doubt an association between nocturnal wanderings and certain conditions, but we don’t know the direction of the causality,” sleepwalking researcher Maurice Ohayon said in a press release. “Are the medical conditions provoking sleepwalking, or is it vice versa? Or perhaps it’s the treatment that is responsible.”
3. There may be a genetic or hereditary component to sleepwalking.
A 2015 study published in the journal JAMA Pediatrics looked at the sleepwalking and sleep terror experiences of 1,940 children. The researchers found that kids with one parent who had ever been a sleepwalker were three times more likely to sleepwalk than kids who had no family history of sleepwalking. When both parents of a child had a history of sleepwalking, the likelihood that their kid would sleepwalk was even higher.
RELATED: Best Mattress For Kids
“With our large cohort, we were able to estimate that children of parents who are or were sleepwalkers are 3 to 7 times more likely to be sleepwalkers themselves depending on whether 1 or both parents had the sleep disorder,” the study authors concluded in the paper.
4. Taking certain medications may increase the likelihood of sleepwalking.
As noted above, people who take SSRI antidepressants may have an increased risk of sleepwalking. Other medications may trigger sleepwalking episodes as well.
In fact, a review of scientific literature published in 2018 found that 29 different medications could be potential triggers for sleepwalking. The drugs belonged to a variety of categories, including benzodiazepine receptor agonists, anti-convulsants, sedative-hypnotics, antidepressants, anti-psychotics, beta blockers, and antibiotics. “Medications can significantly disturb sleep and may trigger sleepwalking in vulnerable people, putting them at risk of injury to themselves and others,” the review concluded.
If someone believes that a medication they take could be triggering sleepwalking episodes, we recommend they speak to the doctor who prescribed the medication to discuss the side effects and see what they recommend. Typically, a person shouldn’t stop taking a prescription medication without their doctor’s go-ahead.
Are you getting enough sleep? See our article on sleep deprivation to know for sure!
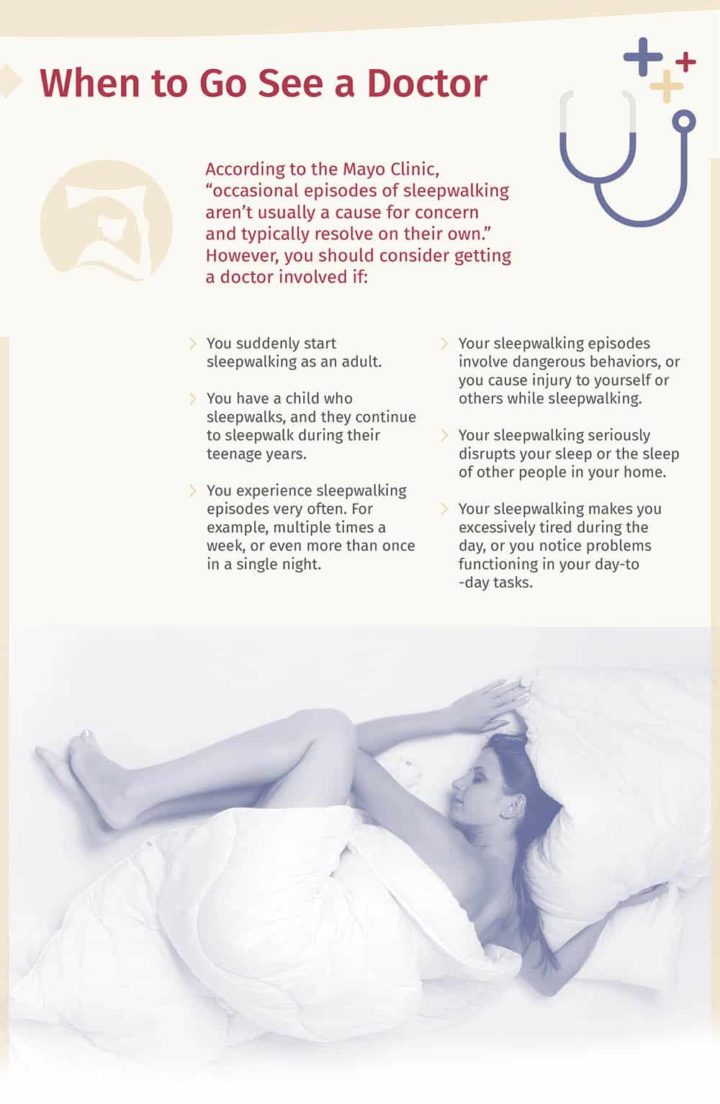
When To See A Doctor For Sleepwalking
People should bring up these issues with their primary care doctor. They may be able to treat the person themselves, or they may refer them to a sleep medicine specialist.
How Is Sleepwalking Diagnosed?
In some cases, sleepwalking may be self-diagnosed. For instance, people who wake up in a different place than the one where they fell asleep, or wake up in the middle of a sleepwalking episode, may find it fairly easy to tell that they were sleepwalking. Self-diagnosis is also possible if someone else witnesses a person sleepwalking.
In other instances, sleepwalkers may be medically diagnosed. The Mayo Clinic website explains that a doctor will examine the patient, chat with them about their symptoms, and review their medical history in order to rule out other conditions and determine whether they qualify for a sleepwalking diagnosis.
Sometimes a doctor might refer their patient to a sleep study, during which they will sleep in a laboratory overnight to see if they sleepwalk. This test, known as a polysomnogram (PSG), monitors a sleeper’s body activity overnight in areas including brain activity, eye movement, heart function, respiration, and muscle movement and tension.
Sleepwalking is not the same as REM Sleep Behavior Disorder (RBD).
In some cases, people may mistake RBD for sleepwalking as they attempt to find a diagnosis for unusual sleep behaviors. But the two conditions are actually quite different.
People who have RBD physically act out their dreams while they are asleep. In contrast, sleepwalkers’ behavior is not informed by their dreams. Most sleepwalking occurs during non-REM sleep, a phase in which dreaming is quite rare.
According to SleepEducation.org, someone acting out their dream due to RBD may do any of the following:
- Shouting
- Swearing
- Flailing
- Grabbing
- Punching
- Kicking
- Jumping
- Leaping
“People with RBD rarely walk, have their eyes open, or leave the room,” the website explains. “These are all common signs of sleepwalking. RBD episodes do not involve eating or drinking. They also do not involve sexual activity or going to the bathroom.”
Other differences between RBD and sleepwalking? It’s usually quite easy to wake someone from an RBD episode, whereas waking a sleepwalker can be difficult. Furthermore, sleepwalkers are often groggy and confused when a person wakes them, and may not understand what’s going on. In contrast, someone woken from RBD episodes is likely to remember vivid details about the dream they were acting out.
RBD is less common than sleepwalking and is most common in men, particularly men over age 50. A meta-analysis of existing research found a connection between RBD and Parkinson’s disease, concluding that “RBD symptoms are common non-motor symptoms of Parkinson’s disease, and people with Parkinson’s disease are at a higher risk of developing RBD.”
Sleepwalking Treatment
In some cases, sleepwalking may resolve without any treatment. For example, it’s very common for children to sleepwalk and then to grow out of it as they get older. A person may not need to seek further treatment for them provided the sleepwalking child doesn’t engage in any troubling behaviors during their sleepwalking episodes.
In other cases, intervention may be necessary in the form of medication and/or natural approaches.
Some people may need medication to counter their sleepwalking.
In some cases, a doctor may decide that a low dose of medication is the appropriate treatment to stop someone from sleepwalking. According to WebMD, doctors may prescribe one of the following medications to treat sleepwalking:
- Estazolam. This is in a class of medication called benzodiazepines, and MedlinePlus says it “works by slowing activity in the brain to allow sleep.” This is a pill one would take at bedtime.
- Clonazepam (Klonopin). This is also a benzodiazepine, which WebMD says “works by calming your brain and nerves.” It is typically used to treat seizures.
- Trazodone (Oleptro). This is in a class of medication called serotonin modulators. Per WebMD, it “works by increasing the amount of serotonin, a natural substance in the brain that helps maintain mental balance.”
That said, since multiple medications have been known to trigger sleepwalking, medication may not be the best choice for many sleepwalkers.
Some natural remedies may help.
According to WebMD, meditation or relaxation techniques may be a natural way to stop sleepwalking.
Another potential remedy that doesn’t involve medication? Hypnosis. Sleep.org explains, “You also might be offered hypnosis, where you are hypnotized and then told to wake up as soon as your feet touch the floor. (The idea is that when you are fast asleep and start to go somewhere, you’ll instantly wake up.)” One study found that hypnosis helped both adults and children who struggled with sleepwalking and nightmares.
Sleepwalking Myths
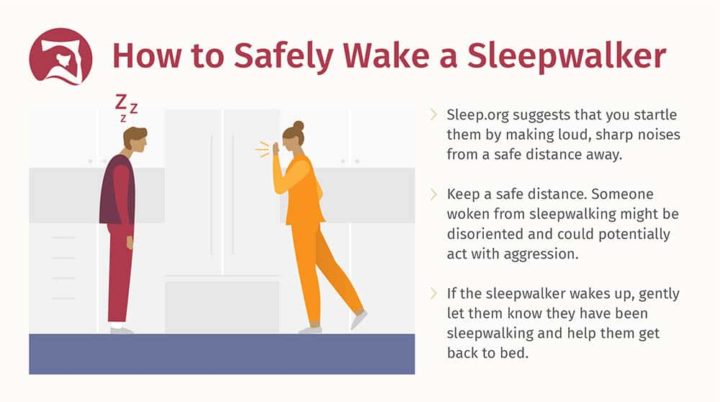
One of the biggest myths about sleepwalking is that witnesses should make every effort to wake a sleepwalker. In reality, that’s not the case. Sleep.org recommends that onlookers try to steer a sleepwalker back to their bed without waking them whenever possible. But in situations where a person can’t get the sleepwalker back into bed, or think they might be a danger to themselves or others, it is recommended to wake a sleepwalker.
Let’s address some other common sleepwalking myths.
Myth: Sleepwalkers act out their dreams.
Reality: As discussed earlier, sleepwalking almost always happens during a non-REM stage of sleep when the person is not actively dreaming. As such, it’s not true that sleepwalkers are acting out their dreams, because they are not dreaming while they sleepwalk.
Myth: People sleepwalk with their eyes closed and their arms out in front of them.
Reality: It’s common to see people sleepwalk like this in movies or television shows. But in reality, sleepwalkers generally have their eyes open so that they can navigate. Their eyes may appear glassy or dazed, but they are open.
Myth: Sleepwalking is the same thing as night terrors.
Reality: A night terror, sometimes known as a sleep terror, is a what happens when “a person… abruptly [awakens] from sleep in a terrified state, but is confused and unable to communicate,” WebMD explains. Usually, people having a night terror won’t respond to voices. The terrors can last anywhere from seconds to minutes, and then the person having them will usually lie down and sleep quietly again. WebMD says people usually don’t remember having night terrors.
According to the Mayo Clinic, people who have night terrors might:
- Suddenly scream or shout in their sleep
- Sit up in their bed, looking scared
- Stare with wide eyes
- Breathe heavily, pant, or hyperventilate
- Have “a racing pulse, flushed face and dilated pupils”
- Thrash or kick
- Be hard to wake up, and seem quite confused if woken up
- Be difficult to console
- Not remember the event the next morning, or remember just a little bit of it
Like sleepwalking, night terrors are more common in children than adults. But night terrors don’t involve getting up, walking around, speaking to others, or other common sleepwalking behaviors.
Myth: Sleepwalking and lucid dreaming are the same.
Reality: Lucid dreaming is still pretty misunderstood, but it’s basically the act of becoming self-aware in your dreams and possibly controlling the action of your dreams.
This is completely different from sleepwalking because sleepwalking rarely involves dreaming, and a sleepwalker has no control over their actions. Plus, according to one Lifehacker article, lucid dreaming happens mostly during REM sleep — unlike sleepwalking, which happens during non-REM sleep. “Lucid dreaming represents a brain state between REM sleep and being awake,” WebMD explains.
How To Prevent Sleepwalking
Depending on what causes the sleepwalking episodes, there are steps a person can take to make sleepwalking less likely:
- If someone sleepwalks because they are stressed, working to eliminate this stress might prevent sleepwalking.
- If someone sleepwalks when they drink alcohol, cutting back on alcohol or not drinking alcohol at all might prevent sleepwalking.
- If someone sleepwalks as a side effect of a medication they are taking, it’s possible that lowering the dosage or going off the medication entirely could prevent sleepwalking. However, patients should always consult their doctor before making any changes to their prescription medications.
The most important thing is to minimize the risk of the sleepwalker harming themselves or others.
Since there is no one proven way to prevent sleepwalking, it’s important that you take steps to keep the sleepwalker as safe as possible. For example:
- Install baby gates at the top of flights of stairs to prevent falling.
- Hide car keys and any weapons at night so the sleepwalker doesn’t have access to them.
- Ensure that windows and doors are securely closed so the sleepwalker can’t wander off.
- Remove clutter to prevent the sleepwalker from tripping over it.
- Ensure that sharp objects are out of reach to prevent accidental harm.
- Put a bell or special sleepwalking alarm on the sleepwalker’s bedroom door at night, so it will ring if they leave their room. This could wake them up or alert other people in the household who can then help the sleepwalker get back into bed.
Evgeny Atamanenko/Shutterstock
Behavioral changes may stop or reduce sleepwalking episodes.
This depends on whether the sleepwalking is related to a particular cause. For example, if a person is sleepwalking as a result of stress, working to mitigate that stress could reduce their sleepwalking. That could mean cutting down on work projects, exercising regularly to lessen stress, or seeing a therapist. If a haphazard sleep schedule is contributing to sleepwalking, sticking to a regular bedtime and wake-up time might reduce the likelihood of sleepwalking.
Experts say that practicing proper sleep hygiene can help you stick to a sleep routine. That means only using your bed for sleep or sex, having some “wind-down” time every night before bed, keeping away from screens before you go to sleep, and sleeping in a cool, dark, quiet room.
If someone notices that they are more likely to sleepwalk after drinking alcohol, it’s possible that reducing or cutting out alcohol consumption could put a stop to their sleepwalking. If you aren’t sure about how to cut down alcohol, talk to your doctor about some potential strategies.
Sleepwalking Summary
Sleepwalking is pretty common, especially in children. In adults, it can be triggered by all sorts of things including medications, fevers, stress, alcohol, and mental health conditions. Most sleepwalkers won’t harm themselves or others, but those who do should seek medical help for the issue — as should people who find that sleepwalking is interfering with their everyday lives. Potential remedies for sleepwalking include medication, stress management, meditation, hypnosis, cutting down on alcohol, and getting adequate, regular sleep.
FAQs
What is sleepwalking?
Sleepwalking is a medical condition formerly known as somnambulism. People with this condition will walk around or perform tasks while they are asleep, though to others they will appear awake.
How do you know when someone is sleepwalking?
Sleepwalkers are known to exhibit some of the following signs of sleepwalking:
- Get out of their bed and walk around the room or house
- Sit up in their bed and open their eyes
- Have a glazed, glassy-eyed expression on their face
- Complete routine daily tasks
- Be difficult to wake up
- Act confused
- Quickly go back to sleep
- Not recall what happened at all
- Experience sleep terrors
Can sleepwalking be treated?
While there is no proven way to prevent sleepwalking, there are various methods to help treat the condition, such as medication, practicing relaxation techniques, and hypnosis among others.
[Editor’s Note: The content provided on this site is for general informational purposes only. Any information provided is not a substitute for professional medical advice. We encourage you to consult with the appropriate health expert if you have concerns.]
Featured image: Africa Studio/Shutterstock